Know more about Caesarean Section (C-section) | Patients & Caregivers
C-Section (Cesarean Section)
Overview
A cesarean delivery, also known as a C-section or cesarean section is the surgical delivery of a baby. It involves one incision in the mother’s abdomen and another in the uterus.
Why a cesarean delivery is done
A cesarean delivery is typically performed when complications from pregnancy make traditional vaginal birth difficult, or put the mother or child at risk. Sometimes cesarean deliveries are planned early in the pregnancy, but they’re most often performed when complications arise during labor.
Reasons for a cesarean delivery include:
- Baby has developmental conditions
- Baby’s head is too big for the birth canal
- The baby is coming out feet first
- Early pregnancy complications
- Mother’s health problems, such as high blood pressure or unstable heart disease
- Mother has active genital herpes that could be transmitted to the baby
- Previous cesarean delivery
- Problems with the placenta, such as placental abruption or placenta previa
- Problems with the umbilical cord
- Reduced oxygen supply to the baby
- Delayed labor
- The baby is coming out shoulder first (transverse labor)
- The mother has a contagious viral infection such as HIV.
The risks of a cesarean delivery
A cesarean delivery is becoming a more common delivery type worldwide, but it’s still a major surgery that carries risks for both mother and child.
The risks of a cesarean delivery include:
- Blood loss
- Blood clots
- Breathing problems for the child, especially if done before 39 weeks of pregnancy
- Increased risks for future pregnancies
- Wound infection
- Injury to the child during surgery
- Longer recovery time compared with vaginal birth
- Surgical injury to other organs
- Adhesions, hernia, and other complications of abdominal surgery
You and your doctor will discuss your birthing options before your due date. Your doctor will also be able to determine if you or your baby are showing any signs of complications that would require a cesarean delivery.
How to prepare for a cesarean delivery
If you and your doctor decide that a cesarean delivery is the best option for you, your doctor will give you complete instructions about what you can do to lower your risk of complications and have a successful cesarean delivery.
As with any pregnancy, prenatal appointments will involve many checkups. This will include blood tests and other examinations to determine your health for the possibility of a cesarean delivery.
Your doctor will make sure to record your blood type in case you need a blood transfusion during the surgery. Blood transfusions are rarely needed during a cesarean delivery, but your doctor will be prepared for any complications.
Even if you aren’t planning to have a cesarean delivery, you should always be prepared for the unexpected. At prenatal appointments with your doctor, discuss your risk factors for a cesarean delivery and what you can do to lower them.
Make sure all of your questions are answered, and that you understand what could happen if you need to have an emergency cesarean delivery before your due date.
Because a cesarean delivery takes additional time to recover than normal birth, arranging to have an extra set of hands around the house will be helpful. Not only will you be recovering from surgery, but your new baby will need some attention as well.
How a cesarean delivery is performed
Plan to stay in the hospital for three to four days while you recover from your surgery.
Before the surgery, your abdomen will be cleaned and you’ll be prepared for receiving intravenous (IV) fluids into your arm. This allows doctors to administer fluids and any type of medications you may need. You will also have a catheter put in to keep your bladder empty during the surgery.
There are three types of anesthesia offered to delivering mothers:
- Spinal block: Anesthesia that’s injected directly into the sac that surrounds your spinal cord, thus numbing the lower part of your body
- Epidural: A common anesthesia for both vaginal and cesarean deliveries, which is injected into your lower back outside the sac of the spinal cord
- General anesthesia: Anesthesia that puts you into a painless sleep, and is usually reserved for emergency situations
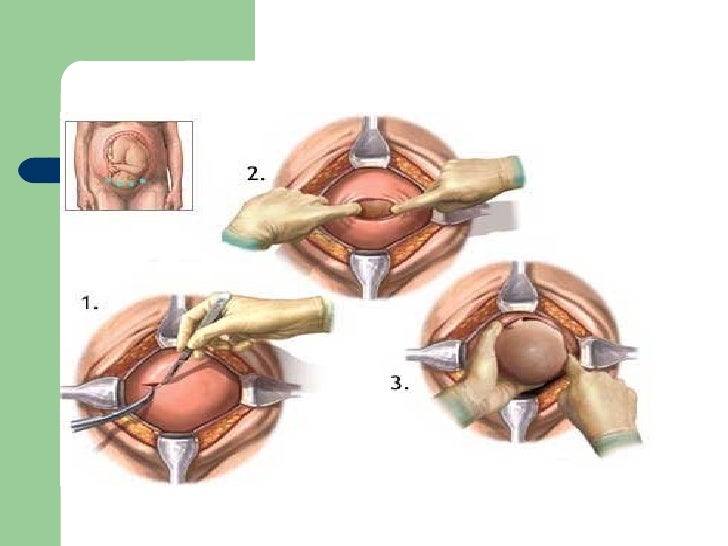
When you have been properly medicated and numbed, your doctor will make an incision just above the pubic hairline. This is typically horizontal across the pelvis. In emergency situations, the incision may be vertical.
Once the incision into your abdomen has been made and the uterus is exposed, your doctor will make an incision into the uterus. This area will be covered during the procedure so you won’t be able to see the procedure.
Your new baby will be removed from your uterus after the second incision is made.
Your doctor will first tend to your baby by clearing their nose and mouth of fluids and clamping and cutting the umbilical cord. Your baby will then be given to hospital staff and they will make sure your baby is breathing normally and prepare your baby to be put into your arms.
Your doctor will repair your uterus with dissolving stitches and close your abdominal incision with sutures.
Following up after a cesarean delivery
After your cesarean delivery, you and your newborn will stay in the hospital for about three days. Immediately after surgery, you will remain on an IV. This allows for adjusted levels of painkillers to be delivered into your bloodstream while the anesthesia wears off.
Your doctor will encourage you to get up and walk around. This can help prevent blood clots and constipation. A nurse or doctor can teach you how to position your child for breastfeeding so there’s no additional pain from the cesarean delivery incision area.
Your doctor will give you recommendations for home care after the surgery, but you should generally expect to:
- Take it easy and rest, especially for the first few weeks
- Use correct posture to support your abdomen
- Drink plenty of fluids to replace those lost during your cesarean delivery
- Avoid sex for four to six weeks
- Take pain medications as needed
- Seek help if you experience symptoms of postpartum depression, such as severe mood swings or overwhelming fatigue
Call your doctor if you experience the following symptoms:
- Breast pain accompanied with a fever
- Foul-smelling vaginal discharge or bleeding with large clots
- Pain when urinating
- Signs of infection — for example, fever over 100°F, redness, swelling, or discharge from the incision






Comments