What Causes Pericarditis?
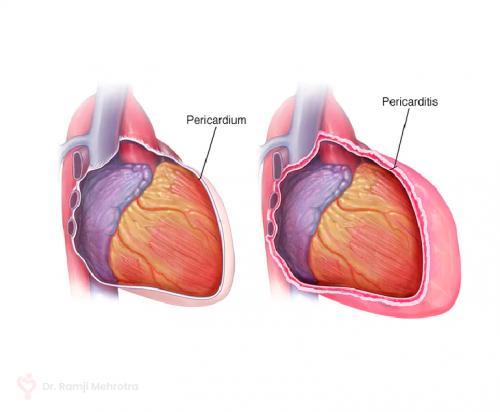
Pericarditis, an inflammatory condition affecting the pericardium - the thin sac-like membrane surrounding the heart, can be a source of acute chest pain and discomfort. While it is often idiopathic or without a known cause, pericarditis can also be triggered by various factors. Understanding these underlying causes is essential for accurate diagnosis, effective treatment, and prevention of recurrence.
Ø Viral Infections: One of the primary causes of pericarditis is viral infections, particularly those caused by the coxsackievirus and echovirus. These viruses can directly invade the pericardium, triggering an inflammatory response. The immune system's reaction to the viral presence can lead to the release of inflammatory chemicals, causing the pericardium to become irritated and inflamed.
Ø Bacterial Infections: While less common, bacterial infections can also result in pericarditis. Bacteria such as Streptococcus, Staphylococcus, and Mycobacterium tuberculosis can infect the pericardium, setting off an inflammatory reaction. Bacterial pericarditis is a more serious condition that requires prompt medical intervention, as it can lead to severe complications.
Ø Autoimmune Disorders: Certain autoimmune disorders can mistakenly direct the immune system to attack healthy tissues, including the pericardium. Conditions like systemic lupus erythematosus (SLE), rheumatoid arthritis, and scleroderma have been associated with an increased risk of developing pericarditis. The immune system's overactivity results in chronic inflammation of the pericardium.
Ø Post-Myocardial Infarction: Pericarditis can arise as a complication following a myocardial infarction (heart attack). The damaged heart tissue releases inflammatory substances that can affect the pericardium. This condition, known as post-myocardial infarction pericarditis, typically occurs within the first few days to weeks after a heart attack.
Ø Trauma or Injury: Physical trauma to the chest, such as from a motor vehicle accident or a fall, can cause inflammation of the pericardium. The trauma might irritate the pericardium directly or indirectly through rib fractures. This form of pericarditis is referred to as traumatic pericarditis.
Ø Medications: Certain medications, particularly those that affect the immune system, can lead to pericarditis as a side effect. Examples include certain anti-seizure medications (phenytoin), immunosuppressive drugs, and medications used to treat tuberculosis (isoniazid).
Ø Radiation Therapy: Individuals who have undergone radiation therapy for chest-related malignancies may develop pericarditis as a late side effect. Radiation can cause inflammation of the pericardium, leading to the development of symptoms over time.
Ø Uremia: Uremia, a condition characterized by high levels of urea and other waste products in the blood due to kidney dysfunction, can lead to pericarditis. The exact mechanisms behind this relationship are not fully understood, but it is believed that the accumulation of waste products in the blood might contribute to inflammation in the pericardium.
Leading cardiovascular surgeon Dr Ramji Mehrotra is of the opinion that in many cases pericarditis is acute and self-limited, meaning it resolves on its own with appropriate treatment. However, it can also become chronic or recur if the underlying cause is not adequately addressed. Diagnosis of pericarditis involves a combination of clinical assessment, medical history review, physical examination, and diagnostic tests such as electrocardiography (ECG), echocardiography, and blood tests to measure markers of inflammation.
Treatment of pericarditis typically involves managing symptoms and addressing the underlying cause. Nonsteroidal anti-inflammatory drugs (NSAIDs) are usually prescribed to reduce inflammation and relieve the pain. In more severe cases, colchicine or corticosteroids might be used. Treating the underlying cause, such as administering antibiotics for bacterial infections or addressing autoimmune conditions, is crucial for preventing recurrence.

Comments